Don’t Fear Rehabbing Patients With Neck Pain
Posted By: Andy Barker
Worry that you might miss something serious…
…worry that you might make your patients symptoms worse or cause more damage…
…uncertainty about what to do if a patient gives you a positive RED FLAG response.
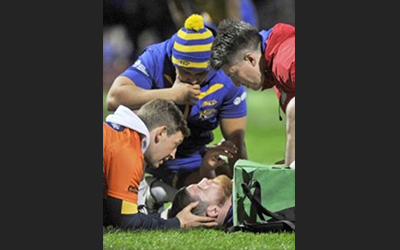
We were all taught about the importance of screening serious injuries during any spinal assessment.
This was drilled into us at Uni…
…and rightly so.
You want and need to make sure that any treatment technique or rehab exercise you prescribe is safe for your patient.
But, the fear of doing more harm or missing something important makes many therapists worry about exactly how to manage injuries like neck pain.
This usually results in a very hands off approach, with therapists being very reluctant to use hands-on treatment techniques and prescribe anything other than very basic rehab exercises.
And this can prevent patient progress and can contribute to patients not making the progress they should.
This blog will help you better understand red flag questioning, learn how to identify which neck pain patients you need to be more cautious with and which patients you can advance more quickly using your hands-on treatment techniques and your rehab.
First…Do No Harm
The first thing you want to do with any injury is to be sure your patient is in the right place.
The neck is no different.
This is where you need to be on the money with your RED FLAG questioning.
Asking these questions helps you determine , first and foremost, if your patient is in the right place.
As therapists it is unlikely we are the first medical practitioner a patient might have seen.
They might have been to see their GP first, then booked an appointment, or been referred via a GP to your NHS clinic for example.
That said, do not take it for granted that a RED FLAG screen has been completed previously or if it has, that it was completed well.
It may well have been, but you need to be sure.
Plus, a patients symptoms might have changed since that consultation.
So it is always good practice to make your own assessment, regardless of what diagnosis or assessment findings are written on the referral letter or the fact your patient tells you they have been given the ‘all clear’ for any serious neck injury.
The first rule of therapy is to first, do no harm.
Unless you complete a good subjective, including RED FLAG questioning, then you will be unsure whether or not the interventions you might use, like any treatments or rehab, will not make your patients symptoms worse.
But what do you do if a patient reports a positive RED FLAG symptom or symptoms?
Why A RED FLAG Does Not Equal No Rehab
The presence of a red flag symptom does not mean that you cannot treat.
The presence of pins and needles or altered sensation does not mean that it is not safe to treat, to use hands-on treatment or prescribe rehab exercises.
We were all taught the importance of RED FLAGS at Uni and why we need to know these questions to identify problems that might be better treated elsewhere…
…but nobody ever told you what to do if a patient presents with less obvious symptoms like some numbness or occasional pins and needles.
If you saw a patient in clinic today that had a history of neck pain and presented with the inability to lift their arm, loss of sensation in their upper limb, problems with their speech or eyesight or difficulty swallowing I think it is clear that you would be suspicion of something sinister.
This is the type of presentation you would be referring quickly to a senior colleague or to A & E.
But patient don’t usually walk into therapy rooms as obvious as this.
Most likely you will be presented with a patient that has less obvious symptoms.
Technically they have positive RED FLAG symptoms.
So, what do you do?
With any type of injury, a patients symptoms will sit on a spectrum, from minimal to major.
This example shows this quite clearly…
A patient may tell they ‘broke their leg.’
This could be a fracture dislocation of their ankle with breaks to both the tibia and fibula or tibial stress fracture.
Both example are fractures and represent a ‘break,’ but clearly they are very different injuries and will require very a different rehab plan.
As long as you are happy that your patient does not have any significant injures that you are think will be made worse by treatment or rehab then you are well placed to help them.
And best of all…
…you can test this out in clinic.
Check If Your Rehab Is ‘Safe’
Patients will often help with this as they will tell you what movements aggravate them and what movements or activities help them.
For example…
A neck pain patient might tell you they get some radiating symptoms down their right arm when they rotate over their right shoulder, like when checking their blind spot when driving…
…but tell you it feels better and the symptoms go away soon as they rotate to the left.
The right rotation might be causing some form of compression or irritation and producing those radicular symptoms.
That could relate to the cervical discs or facet joints.
The fact they told you movement the opposite way helps, is very useful and would be a good place to start.
Maybe some mobility work including left rotation or left side flexion might help to decompress and open up their affected right side.
Given your patient has already told you it helps their symptoms it would be logical to think that this movement to the left might help.
The easiest bit…
You can test this.
Just do the exercise i.e. left side flexion or your treatment technique and then retest.
Choose one of your objective markers, test it, do your treatment or rehab, then re-test it.
If it improves patient symptoms then you can be confident that you will not be doing any harm to your patient treating their neck and at the same time you can give them rehab you know is helping their symptoms.
Key Points
First…Do No Harm: Use your subjective and your RED FLAG questions to clear any significant and possible sinister injuries. If in doubt refer on to a senior colleague or to A & E.
Why A RED FLAG Does Not Equal No Rehab: Providing you are happy you are not dealing with a sinister neck injury, treatment and rehab will likely help your patients pain and like any other injury, is likely needed to help them get back to full function.
Check If Your Rehab Is ‘Safe’: Use a test-intervention-retest method to ensure any treatment technique or rehab exercise you prescribe are both safe and will help your patient with their neck symptoms.
The New Grad Physio Mentor
PS. Do you struggle with neck pain patients?
I’d love to hear what you struggle with and to help you out overcoming these problems, specific to the neck, to give you greater confidence with your neck patient assessments and rehab.
Email me at andy@newgradphysio.com and I’ll let you know a couple of really simple ways in which to do this…