Don’t Treat The MRI…
Posted By: Andy Barker
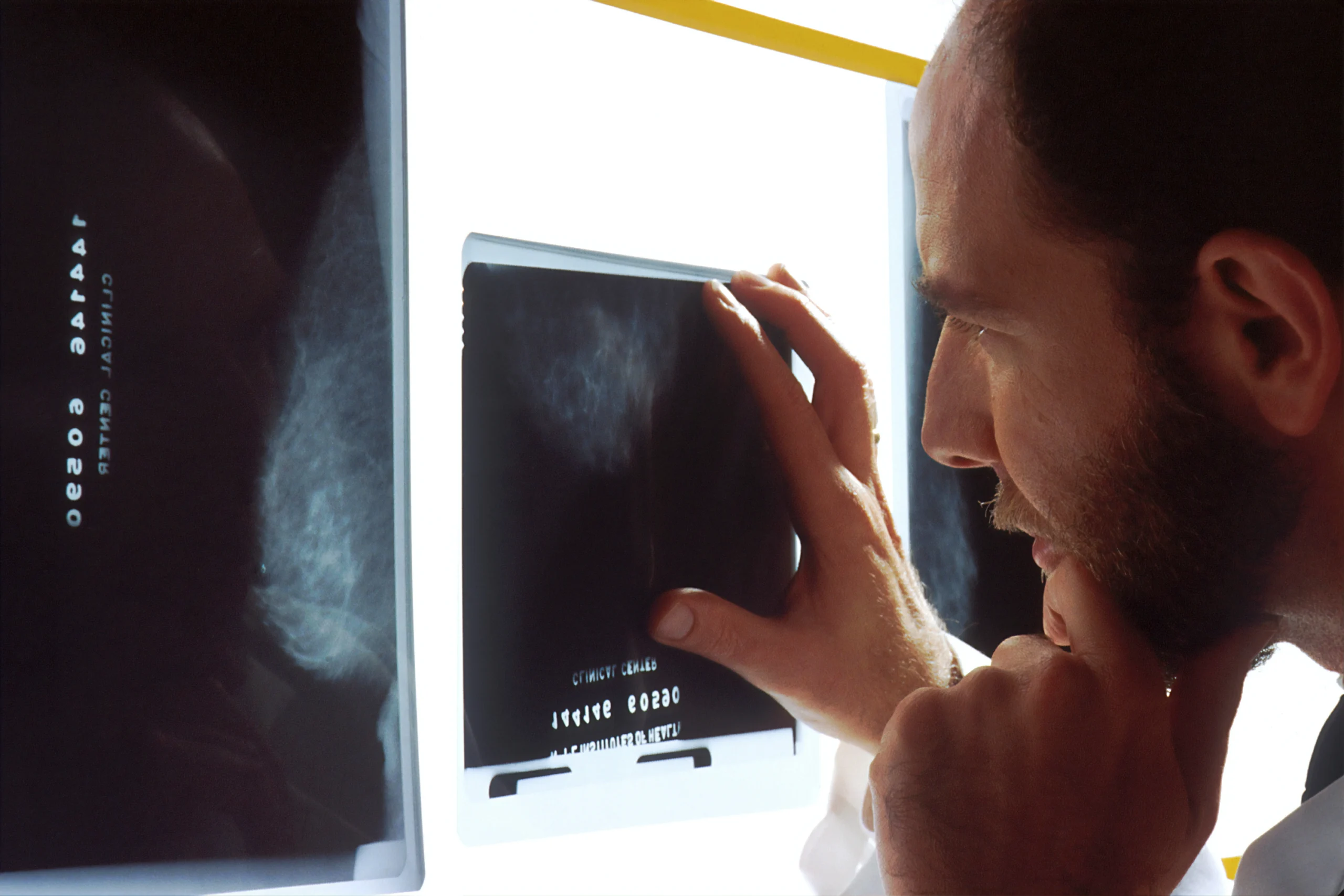
Whether that’s an MRI, ultrasound, x-ray or CT scan they are great tools…
But they are just that…a tool.
They are part of your ‘diagnostic toolbox’ and go alongside your clinical assessment to help identify a patient’s problem or problems so you can ensure they are being managed in the best possible way.
At no point should imaging replace your clinical assessment.
And at no point should imaging results determine solely your management of any patient you are working with.
I had a problem just this week with a professional rugby player I was working with.
He had picked up a valgus type injury, fixed foot with his knee forced into valgus under load, and tested like an MCL, showing a high degree of laxity on clinical testing.
He also presented with increased laxity on ACL and PCL testing, so with the MCL and other findings I referred him for an MRI.
However, the MRI findings were very different to how he presented on the bed.
When there is a difference between clinical finding and radiological finding’s we should question why this is.
And that’s what I did.
I asked for the scan to be re-read and the second time around it showed different results.
This made more sense as it linked to how he presented on the bed.
This example goes to show how clinical findings can differ from radiological findings and why we should consider imaging as just ONE tool in our toolkit and NOT the diagnostic holy grail that is sometimes seen as.
Failure to do this can cause big problems, as therapists sometimes treat the scan and NOT the patient’s actual problems.
In a very similar way, you might sometimes second guess yourself when you find different problems with your patient to their given ‘diagnosis’ from another practitioner, like a GP.
You may get that referral from a GP or consultant for a patient that has been referred for physio and in most cases like this, the patient has already been given a diagnosis.
Your referral letter probably even has it at the top of the letter in bold!
What happens here is that you just end up treating the problem on the referral letter or the findings of the MRI report, even though it might be different from the problems you identify during your own clinical assessment.
In the remainder of this blog I want to go into more detail about three main themes…
The 3 Reasons You Should Refer A Patient For Imaging
Discuss If You Should Refer Muscle Injuries For Imaging
Cover The Problem With Current Injury Grading Classifications & Why Some Patients Get The Wrong Interventions As A Result
When To Refer For Imaging?
You need to consider imaging for 1 of 3 reasons;
1) To Rule Out Sinister Pathology
If something doesn’t appear that it is your field i.e. not MSK and/or the patient presents with red flags your patient may warrant further investigation.
In most cases as a junior physio it might be that you refer to another practitioner first, then they may consider onward referral for imaging.
2) It Is Unclear What The Specific Injury Is
This can be common in acute injuries where-by you may be unable to objectively test your patient because of pain, inflammation or apprehension.
In cases like this imaging can be helpful.
3) You Suspect Your Patient Needs Further Intervention
For example, if you suspected an ACL, fracture or a traumatic shoulder labral tear and you think it’s likely your patient may need referral to see a consultant or need further intervention, i.e. surgery, then imaging is warranted.
Should You Scan Muscle Injuries?
In short, no.
Most muscle injuries don’t need imaging.
With any injury, always ask yourself the question;
Will the imaging help your management of this patient or athlete?
Would the result of a grade 1 or grade 2 hamstring injury on an MRI greatly change your management of your patient or athlete?
I would say no, as your rehab progressions are always going to be led by how your patient tests in clinic and by your objective testing.
The only time imaging for muscle injuries may be warranted is if you thought there may be a tendon injury and as a result this may change your management approach e.g. possible surgery warranted in severe cases.
What Grade Injury Is It?
Traditional grading systems are almost a thing of the past…
Grade 1-3 scales do have limitations.
Take a Grade 2 injury for example.
A Grade 2 injury indicates that there is more than 10% of fibres involved in the injury but less than 99.9% of fibres involved.
A patient or athlete with 99.9% of fibre involvement tells us that the tendon is still attached, hence it is not a Grade 3 injury, but clearly an injury like this is very different to an injury to the same muscle that has only 11% of fibres injured.
This has led to the development of newer injury classification grading systems like the BAMIC system developed by British Athletics.
These are much more detailed and almost force radiologists to be more specific when reporting muscle injuries.
The BAMIC system also helps to differentiate muscle injuries that do or don’t have tendon involvement, which as mentioned above, helps us to consider if the best way to manage an injury is conservatively or not.
That said, even using more detailed injury grading systems have limitations.
I still think some muscle injuries are sent too early for surgery and not given chance for conservative management.
A Grade 3C muscle injury on the BAMIC system would indicate that there is 50% tendon involvement, but the tendon is still attached.
Many cases like this are sent for immediate surgery.
On the traditional grading systems this injury would be classified as a Grade 2.
Maybe medical professionals are seeing the number ‘3’ and are comparing this to the old school grading system, where a grade 3 would be a complete rupture (tendon detached from the bone)…
I’m not sure, but whatever it is we are seeing more and more surgical interventions for muscle injuries when the tendon is still intact.
I’m not saying this is right or wrong, as EVERY case should be considered invidually.
But what I am saying is that imaging is just ONE tool in your toolbox…
Key Points
When Should You Refer For Imaging – To Rule Out Sinister Pathology OR If The Injury Is Unclear &/Or You Are Unable To Test OR If Surgery Is A Likely Outcome
Should You Image Soft Tissue Injuries? – In Short NO, Unless There Is Tendon Involvement
The Problem With Grading Classifications – Traditional Systems Are Basic, But Even More Detailed Systems Need To Be Used In COMBINATION With Clinical Findings To Judge The Best Course Of Management For That Injury
I would love to hear your experiences with imaging.
Have you seen cases where your clinical findings don’t match the radiological findings?
Do you find yourself sometimes treating the scan (or the referral letter) and NOT the patient?
Reach out to me at andy@newgradphysio.com
Andy Barker
The New Grad Physio Mentor