Taking The Fear Away From Treating Neck Pain Patients
Posted By: Andy Barker
Do you worry when a neck injury patient walks in your clinic?
Do you worry that you might miss something serious…
…or that you might make your patients symptoms worse or cause more damage?
Maybe it’s the uncertainty about what to do if a patient gives you a positive response to one of your red flag questions.
Whatever it is it’s not great and affects your ability to help your patient.
This problem in large stems from some of scaremongery that happens at University.
It was drilled into you at Uni that you need to screen for serious injuries during any spinal assessment…
…and rightly so.
Before you get consider getting your hands-on or giving rehab exercises to any patient you of course need to be sure that it is safe to do so.
But even when you do this and having completed your assessment and you are happy they are safe…
Many therapists still fear doing more harm to their patient or still have that lingering doubt that they have missed something with the neck.
The most common result of this is that you do very little or even worse…
Tell your patient to ‘rest’ because you fear doing more harm than god with your interventions.
Sound like you?
One thing you need to understand is that almost all patients NEED hands-on or rehab, usually both.
So your hands-on off approach can be detrimental and can actually prevent a patient’s improvement both in pain and function.
One of the biggest misconceptions with neck pain is that the presence of a red flag means a hands-off approach.
The presence of a red flag symptom does not mean that you cannot treat your patient or give a patient rehab.
The presence of neural symptoms into the arm like pins and needles or altered sensation is common for patients with neck pain…
And is a red flag symptom.
But are you sending this patient straight to A & E?
I hope you are not.
These patients are really common and more often than not, they will respond quickly to treatment and rehab, if you use the right techniques and give them the right exercises.
Just think about what a nerve actually likes.
Nerves like movement, space and a rich blood supply…
Just like a muscle.
You know that ‘rest is NOT best, for muscle injuries, so why would you prescribe this approach to nerve injuries?
It makes no sense!
As long as you are happy that your patient does not have any significant injures they are safe in your care.
I covered a neck case study last week in the members group of my new grad physio membership.
This female patient had initially started with neck pain, which followed by the onset of some radiating symptoms down the back of her arm and into her hand.
Every Monday I post a case study in the group so that the therapists can take a look and clinically reason how they would manage this type of problem themselves.
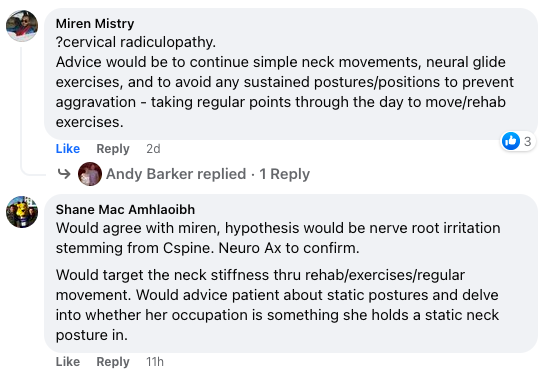
Just like Miren & Shane…
Every Friday I then do a live video in the group where I go through the case study in detail and give my reasons for the diagnosis and what treatment and rehab I used for this specific patient.
One of the big advantages of this is that you get to see injuries that you might not have been covered at University or had the experience of seeing before.
This gives you the chance to clinically reason what you might do if you were presented with a similar patient…
Without having to try work it out for the first time on the fly with a real patient stood right in front of you in clinic!
These are real patients seen in the clinic or athletes I have been working with, not made up case studies like you ‘treated’ at Uni.
This is key…
As how you were told patients will report symptoms during the assessment at University is very different to how they actually present in real life!
Andy
The New Grad Physio Mentor
PS. Do you struggle with neck pain patients?
If you would like to build greater confidence with your neck patient assessments, treatments and rehab…And get the support you need to put these skills into practice with patients in the real world then head here to find out how!